Authored by Marina Zhang via The Epoch Times (emphasis ours),
Cases of a rare autoimmune disease surged between 2020 and 2022 in Yorkshire, England, peaking in 2021. COVID-19 infection and its vaccines possibly contributed to the rise, a recent study in The Lancet’s eBioMedicine found.
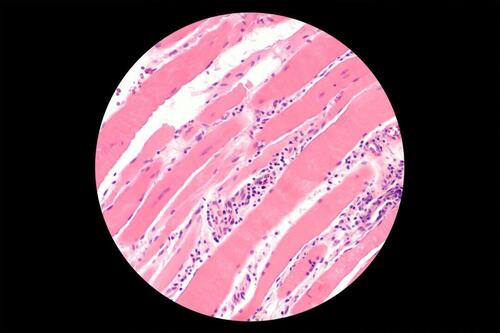
The disease—melanoma differentiation-associated protein-5 (anti-MDA5) positive dermatomyositis, or anti-MDA5 dermatomyositis—is an inflammatory disease characterized by muscle weakness, skin rashes, and rapidly progressive lung disease.
Anti-MDA5 dermatomyositis is very rare.
In 2019, Yorkshire, which has a population of 3.6 million, reported two people testing positive for the disease. In 2020, there were nine. Cases peaked in 2021 with 35 new cases. The number then dropped to 16 new cases in 2022.
The new autoimmune cases may have arisen from the COVID-19 virus and vaccine RNA interactions, the study’s senior author, Dr. Dennis McGonagle, clinical professor of medicine at the University of Leeds, told The Epoch Times.
Besides the Lancet study, several case studies have documented new anti-MDA5 cases following COVID-19 infection or vaccination.
What Is Anti-MDA5 Dermatomyositis
Anti-MDA5 dermatomyositis is an autoimmune condition in which the body attacks itself. It can often appear without a clear cause.
Dermatomyositis tends to affect the skin, muscles, and lungs. Anti-MDA5 dermatomyositis involves rapidly progressive lung disease, which lends the condition a poor prognosis.
MDA5 is a protein present outside of muscles and tissues, especially prominent in the lungs. Therefore, when the body forms anti-MDA5 antibodies to attack MDA5, it can deteriorate related organs and tissues.
MDA5 can detect and bind to foreign RNA, including COVID-19 RNA. Upon detection, it signals other immune cells to fight the foreign invader or vaccination.
“We think that ... [this happens] because MDA5 is the receptor or docking site for viral RNA, and that this in some way triggers the antibody against it,” Dr. McGonagle said.
In a COVID-19 infection, MDA5’s binding to RNA can result in too much MDA5 activity as a response, Dr. Pradipta Ghosh, director of the Institute for Network Medicine at the University of California–San Diego and another corresponding author of the study, told The Epoch Times.
COVID-19 patients were shown to have high MDA5 gene activity in their lung fluids, further suggesting that the virus might have triggered new MDA5 cases.
Apart from anti-MDA5, 15 other autoantibodies can contribute to similar dermatomyositis diseases. The role of MDA5 in COVID-19 infection and vaccination may explain why, during the pandemic, only anti-MDA5 dermatomyositis cases increased while other autoantibodies involved in dermatomyositis did not.
Between 2020 and 2022, all 60 new anti-MDA5 dermatomyositis patients in Yorkshire were evaluated. All developed symptoms.
Over 40 percent developed interstitial lung disease and had a worse prognosis. Half died by the time the study was published.
The authors noted that anti-MDA5 cases during the pandemic presented slightly differently than pre-pandemic cases.
Compared to pre-pandemic, anti-MDA5 cases reported during the pandemic had a lower rate of lung disease and a lower death rate, said Dr. Ghosh. The disease also affected white people as opposed to Asians, who were the more predominant demographic previously.
Pandemic-era patients tend to report skin-related conditions such as rashes, decreased blood flow to fingers, muscle aches, and so on.
Coincidental Rise
The peak of anti-MDA5 cases between April and July 2021 coincided closely with Yorkshire’s uptake of COVID-19 vaccines and occurred during a time of “higher community SARS-CoV-2 positivity during 2021,” the authors reported. Vaccinations started in Yorkshire in January 2021 and dropped off in October.
Around 90 percent of the Yorkshire population was vaccinated, and 49 of the 60 cases had documented COVID-19 vaccination.
Contrastingly, only 15 out of 60 had had a confirmed COVID-19 infection.
While many people tested positive for COVID-19 at the time, the authors noted that anti-MDA5 cases did not rise immediately after a rise in COVID-19 cases.
Other Reports
In addition to the reports in Yorkshire, other studies have shown a link between anti-MDA5 dermatomyositis and COVID-19 and its vaccine.
An Italian case study published in Frontiers in Immunology reported the case of an older, unvaccinated woman who developed anti-MDA5 dermatomyositis a month after her COVID-19 infection. She had joint pain and developed rashes and lesions on her chest, face, and hands.
The authors argued that MDA5, which is involved in the activation of various cytokines, may precipitate inflammatory reactions when exposed to SARS-CoV-2.
Another paper published in SN Comprehensive Clinical Medicine reported an anti-MDA5 dermatomyositis case that occurred a week after COVID-19 vaccination. The researchers hypothesized that antibodies to spike proteins on the SARS-CoV-2 virus may cross-react with human proteins like MDA5.
However, Dr. Ghosh said that while spike protein has been implicated in other autoimmune diseases, anti-MDA5 disease is caused by antibodies against MDA5, not spike.
“I believe that we have a lot of work to do before we can begin to understand why or how our body responds to this virus, its particles, its RNA/protein—even the RNA encoding its key components we use as vaccine in the plethora of ways that it does,” she explained.
Authored by Marina Zhang via The Epoch Times (emphasis ours),
Cases of a rare autoimmune disease surged between 2020 and 2022 in Yorkshire, England, peaking in 2021. COVID-19 infection and its vaccines possibly contributed to the rise, a recent study in The Lancet’s eBioMedicine found.
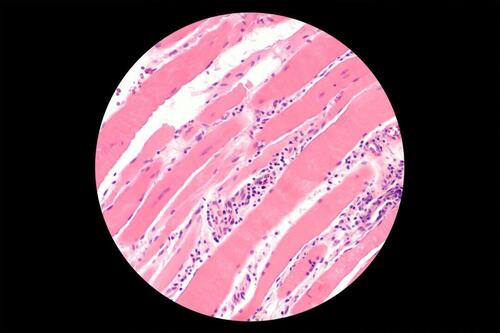
The disease—melanoma differentiation-associated protein-5 (anti-MDA5) positive dermatomyositis, or anti-MDA5 dermatomyositis—is an inflammatory disease characterized by muscle weakness, skin rashes, and rapidly progressive lung disease.
Anti-MDA5 dermatomyositis is very rare.
In 2019, Yorkshire, which has a population of 3.6 million, reported two people testing positive for the disease. In 2020, there were nine. Cases peaked in 2021 with 35 new cases. The number then dropped to 16 new cases in 2022.
The new autoimmune cases may have arisen from the COVID-19 virus and vaccine RNA interactions, the study’s senior author, Dr. Dennis McGonagle, clinical professor of medicine at the University of Leeds, told The Epoch Times.
Besides the Lancet study, several case studies have documented new anti-MDA5 cases following COVID-19 infection or vaccination.
What Is Anti-MDA5 Dermatomyositis
Anti-MDA5 dermatomyositis is an autoimmune condition in which the body attacks itself. It can often appear without a clear cause.
Dermatomyositis tends to affect the skin, muscles, and lungs. Anti-MDA5 dermatomyositis involves rapidly progressive lung disease, which lends the condition a poor prognosis.
MDA5 is a protein present outside of muscles and tissues, especially prominent in the lungs. Therefore, when the body forms anti-MDA5 antibodies to attack MDA5, it can deteriorate related organs and tissues.
MDA5 can detect and bind to foreign RNA, including COVID-19 RNA. Upon detection, it signals other immune cells to fight the foreign invader or vaccination.
“We think that ... [this happens] because MDA5 is the receptor or docking site for viral RNA, and that this in some way triggers the antibody against it,” Dr. McGonagle said.
In a COVID-19 infection, MDA5’s binding to RNA can result in too much MDA5 activity as a response, Dr. Pradipta Ghosh, director of the Institute for Network Medicine at the University of California–San Diego and another corresponding author of the study, told The Epoch Times.
COVID-19 patients were shown to have high MDA5 gene activity in their lung fluids, further suggesting that the virus might have triggered new MDA5 cases.
Apart from anti-MDA5, 15 other autoantibodies can contribute to similar dermatomyositis diseases. The role of MDA5 in COVID-19 infection and vaccination may explain why, during the pandemic, only anti-MDA5 dermatomyositis cases increased while other autoantibodies involved in dermatomyositis did not.
Between 2020 and 2022, all 60 new anti-MDA5 dermatomyositis patients in Yorkshire were evaluated. All developed symptoms.
Over 40 percent developed interstitial lung disease and had a worse prognosis. Half died by the time the study was published.
The authors noted that anti-MDA5 cases during the pandemic presented slightly differently than pre-pandemic cases.
Compared to pre-pandemic, anti-MDA5 cases reported during the pandemic had a lower rate of lung disease and a lower death rate, said Dr. Ghosh. The disease also affected white people as opposed to Asians, who were the more predominant demographic previously.
Pandemic-era patients tend to report skin-related conditions such as rashes, decreased blood flow to fingers, muscle aches, and so on.
Coincidental Rise
The peak of anti-MDA5 cases between April and July 2021 coincided closely with Yorkshire’s uptake of COVID-19 vaccines and occurred during a time of “higher community SARS-CoV-2 positivity during 2021,” the authors reported. Vaccinations started in Yorkshire in January 2021 and dropped off in October.
Around 90 percent of the Yorkshire population was vaccinated, and 49 of the 60 cases had documented COVID-19 vaccination.
Contrastingly, only 15 out of 60 had had a confirmed COVID-19 infection.
While many people tested positive for COVID-19 at the time, the authors noted that anti-MDA5 cases did not rise immediately after a rise in COVID-19 cases.
Other Reports
In addition to the reports in Yorkshire, other studies have shown a link between anti-MDA5 dermatomyositis and COVID-19 and its vaccine.
An Italian case study published in Frontiers in Immunology reported the case of an older, unvaccinated woman who developed anti-MDA5 dermatomyositis a month after her COVID-19 infection. She had joint pain and developed rashes and lesions on her chest, face, and hands.
The authors argued that MDA5, which is involved in the activation of various cytokines, may precipitate inflammatory reactions when exposed to SARS-CoV-2.
Another paper published in SN Comprehensive Clinical Medicine reported an anti-MDA5 dermatomyositis case that occurred a week after COVID-19 vaccination. The researchers hypothesized that antibodies to spike proteins on the SARS-CoV-2 virus may cross-react with human proteins like MDA5.
However, Dr. Ghosh said that while spike protein has been implicated in other autoimmune diseases, anti-MDA5 disease is caused by antibodies against MDA5, not spike.
“I believe that we have a lot of work to do before we can begin to understand why or how our body responds to this virus, its particles, its RNA/protein—even the RNA encoding its key components we use as vaccine in the plethora of ways that it does,” she explained.
